doi: 10.56294/shp2024121
SYSTEMATIC REVIEW
Impact of contrast agents on renal function: a systematic review
Impacto de los agentes de contraste en la función renal: revisión sistemática
Aline Aparecida Pacheco1 ![]() *, Analía Claudia Sabattini1
*, Analía Claudia Sabattini1 ![]() *
*
1Universidad Abierta Interamericana, Facultad de Medicina y Ciencias de la Salud, Carrera de Medicina. Buenos Aires, Argentina.
Cite as: Pacheco AA, Sabattini AC. Impact of contrast agents on renal function: A systematic review. South Health and Policy. 2024; 3:121. https://doi.org/10.56294/shp2024121
Submitted: 03-08-2023 Revised: 24-12-2023 Accepted: 16-06-2024 Published: 17-06-2024
Editor:
Dr. Telmo Raúl Aveiro-Róbalo ![]()
Corresponding Author: Analía Claudia Sabattini *
ABSTRACT
Introduction: radiological contrast agents are essential for obtaining accurate medical images; however, their use carries a significant risk of nephrotoxicity, a complication that can lead to acute kidney injury (AKI). This systematic review aims to assess the impact of iodinated and gadolinium-based contrast agents on kidney function, comparing their relative risk of inducing contrast-induced nephropathy (CIN).
Objective: to evaluate the impact of radiological contrast agents on renal function.
Method: a systematic review of the literature available in databases such as PubMed and Google Scholar were conducted. Observational studies controlled clinical trials, meta-analyses, and systematic reviews published between 2009 and 2024 that evaluated the impact of iodinated and gadolinium-based contrast agents in adult patients undergoing imaging studies were included.
Results: the review indicated that the incidence of contrast-induced nephropathy (CIN) varies according to the type of contrast agent and patient conditions. In populations without risk factors, the incidence of CIN was low, while in patients with chronic kidney disease or diabetes, the incidence was significantly higher (up to 12 %). No significant differences were observed between iodinated and gadolinium-based contrast agents in terms of CIN risk. In patients with renal insufficiency, proper hydration, combined with other measures such as the use of nitrates, was highlighted as the most effective preventive strategy. There was no clear benefit of N-acetylcysteine in reducing CIN. Overall, intravenous hydration remains the key preventive measure to reduce CIN risk.
Conclusions: the literature review indicates the need for more rigorous clinical trials to assess the efficacy and safety of different contrast agents. It highlights the importance of a thorough assessment of individual risk factors to minimize nephrotoxicity in patients undergoing contrast-based procedures.
Keywords: Contrast Media; Iodine; Gadolinium; Acute Kidney Injury; Diagnostic Imaging; Intravascular Administration.
RESUMEN
Introducción: los agentes de contraste radiológico son fundamentales para la obtención de imágenes médicas precisas; sin embargo, su uso conlleva un riesgo significativo de nefrotoxicidad, una complicación que puede derivar en insuficiencia renal aguda (IRA). Esta revisión sistemática se propone evaluar el impacto de los agentes de contraste yodados y basados en gadolinio sobre la función renal, comparando su riesgo relativo de inducir nefropatía por contraste (NIC).
Objetivo: evaluar el impacto de los agentes de contraste radiológico en la función renal.
Método: se llevó a cabo una revisión sistemática de la literatura disponible en bases de datos como PubMed y Google Académico. Se incluyeron estudios observacionales, ensayos clínicos controlados, metaanálisis y revisiones sistemáticas publicados entre 2009 y 2024 que evaluaran el impacto de los contrastes yodados y basados en gadolinio en pacientes adultos sometidos a estudios de imagen.
Resultados: la revisión de los estudios indicó que la incidencia de nefropatía inducida por contraste (NIC) varía según el tipo de agente de contraste y las condiciones de los pacientes. En poblaciones sin factores de riesgo, la incidencia de NIC fue baja, mientras que, en pacientes con insuficiencia renal crónica o diabetes, la incidencia fue significativamente mayor (hasta 12 %). No se observaron diferencias relevantes entre el uso de contrastes yodados y basados en gadolinio en cuanto a riesgo de NIC. En pacientes con insuficiencia renal, la hidratación adecuada, combinada con otras medidas como el uso de nitratos, se destacó como la estrategia preventiva más eficaz. No se observó un beneficio claro de la N-acetilcisteína en la reducción de NIC. En general, la hidratación intravenosa sigue siendo la medida preventiva clave para reducir el riesgo de NIC.
Conclusiones: la revisión de la literatura indica la necesidad de realizar ensayos clínicos más rigurosos para evaluar la eficacia y seguridad de los distintos agentes de contraste. Se subraya la importancia de una evaluación minuciosa de los factores de riesgo individuales con el fin de reducir al mínimo la nefrotoxicidad en pacientes que se someten a procedimientos con medios de contraste.
Palabras clave: Medios de Contraste; Yodo; Gadolinio; Lesión Renal Aguda; Diagnóstico por Imagen; Administración Intravascular.
INTRODUCTION
Contrast agents, both iodinated and gadolinium-based, have been fundamental in various diagnostic procedures. Iodinated contrasts, frequently used in computed tomography (CT) and angiography, significantly improve the visualization of blood vessels and organs, which is key to accurately detecting various pathologies, especially cardiovascular and neoplastic ones. Similarly, gadolinium-based contrast agents, used primarily in magnetic resonance imaging (MRI), are essential for more clearly differentiating soft tissues and facilitating the identification of lesions in the brain, spinal cord, and liver. Their use is approved for patients with specific indications, such as suspected tumors or vascular diseases. However, their administration must be preceded by a rigorous assessment of renal function, especially in patients with chronic renal failure or diabetes, due to the risk of developing contrast-induced nephropathy. Current recommendations emphasize the importance of this careful assessment to minimize potential risks.(1)
However, the use of these agents is not without risks, with nephrotoxicity being one of the most concerning adverse effects. Contrast-induced nephropathy (CIN) refers to the deterioration of kidney function after exposure to these agents, typically manifesting as an increase in serum creatinine levels within 24 to 72 hours.
The mechanisms underlying CIN include renal vasoconstriction, free radical generation, and direct damage to renal tubular cells. These mechanisms lead to renal ischemia, oxidative stress, and cell death, compromising renal function. Recent literature has emphasized that both iodinated agents, used in CT, and gadolinium-based agents, used in MRI, can induce nephrotoxicity, especially in patients with preexisting risk factors such as chronic kidney disease and diabetes.(2)
The incidence of CIN varies significantly depending on the type of contrast agent and the population studied. Although low-osmolar contrast agents have been shown to reduce the risk of CIN compared to their high-osmolar counterparts, the risk remains considerable in patients with pre-existing renal impairment. In this context, the appropriate selection of contrast agents and the implementation of preventive strategies such as hydration is crucial to minimize the risk of CIN. Hydration improves renal blood flow and dilutes the contrast agent within the renal tubules. As a result, the concentration of contrast is reduced, decreasing its toxic potential and protecting kidney cells from possible ischemic and oxidative damage. Hydration is recommended by the European Society of Urogenital Radiology (ESUR) guidelines, as it also facilitates faster elimination of contrast through the kidneys, reducing exposure time and, consequently, the risk of adverse effects.(3)
Some studies have shown that iso-osmolar agents, such as iodixanol, have a reduced risk of nephrotoxicity compared to other low-osmolarity agents. This approach particularly benefits patients with impaired renal function, reducing the osmotic load and decreasing the risk of induced kidney damage.(4)

Figure 1. Oxidative stress mechanisms related to contrast-induced nephropathy
METHOD
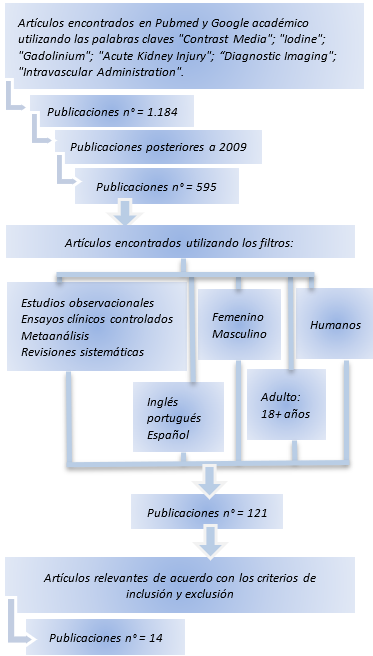
Figure 2. Flow Chart 1. Process for identifying included studies
Study design
This study was structured as a systematic review whose main objective was to investigate the risk of contrast-induced nephropathy (CIN) in different types of radiological contrast media. The review evaluated CIN in patients who received iodinated or gadolinium-based contrast media, paying special attention to preventive strategies to mitigate these risks.
A thorough search was conducted in recognized databases such as PubMed and Google Scholar. The keywords used included “Contrast Media,” “Iodine,” “Gadolinium,” “Acute Kidney Injury,” “Diagnostic Imaging,” and “Intravascular Administration.” To maximize the retrieval of relevant studies, Boolean operators (AND, OR) were applied to effectively combine these terms. The search was limited to publications between 2009 and 2024, and studies available in English, Spanish, and Portuguese were included.
Inclusion criteria
· Studies report the incidence of CIN in adult patients exposed to iodinated or gadolinium-based contrast media.
· Controlled clinical trials, observational studies, systematic reviews, and meta-analyses.
· Publications between 2009 and 2024 (15 years)
· Studies addressing contrast-induced nephropathy (CIN) and including analysis of variables such as:
1. Infusion rate, total volume administered.
2. Type of contrast agent used.
3. Implementation of pre- and post-procedure hydration strategies.
4. Use of pharmacological agents.
5. Monitoring of renal function.
Exclusion criteria
· Research that does not specify the type of contrast medium used.
· Research that does not provide conclusive data for the investigation.
· Studies that focus solely on pediatric or pregnant populations unless they include a separate and detailed analysis of adult patients.
· Preclinical studies and opinion articles were excluded from the review.
Study Selection
The articles obtained were subjected to a multi-stage selection process. Initially, a review of the titles and abstracts was conducted to identify studies that aligned with the specific objectives of the research. Articles that passed this stage were evaluated to determine their compatibility with the previously established selection criteria.
Key data were extracted from the selected studies, such as study design, population characteristics, interventions applied (including hydration measures and type of contrast medium used), main results in relation to the incidence of CIN, and limitations identified in each study.
The data were synthesized using narrative methods and systematically recorded in a pre-established sheet designed to store and organize the relevant information from each study. This approach facilitated the identification of patterns and trends in CIN and the evaluation of preventive strategies. A descriptive analysis of the results was performed, which allowed the identification of CIN patterns according to the type of contrast medium, the preventive strategy applied, and the risk factors present in the population.
RESULTS
|
Table 1. Presentation of results |
||||||
|
Author(s) |
Type of study |
Patient Characteristics and Number |
Type of contrast |
Contrast-induced nephropathy |
Preventive Strategies |
Main Results |
|
Gorelik et al.(4) |
Retrospective clinical study |
12 580 patients underwent computed tomography with iodinated contrast and 754 patients underwent magnetic resonance imaging with gadolinium |
Iodinated contrast (Iohexol) and gadolinium (Gadoterate meglumine) |
7,3 % in patients with gadolinium versus 8 % in patients with iodinated contrast; after propensity score matching: 7 % (not significant) |
Hydration and blood pressure control |
The risk of contrast-induced nephropathy was similar between iodinated and gadolinium-based contrast agents after adjusting for risk factors |
|
McDonald et al.(5) |
Retrospective clinical study |
157 140 scans in 53 439 patients, comparing computed tomography with and without contrast |
Iodinated contrast (Omnipaque and Visipaque) |
There was no significant difference in the risk of acute kidney injury between the contrast and non-contrast groups after adjustment for propensity score |
Adjustment for risk factors using propensity scoring |
There was no evidence that intravenous contrast caused significantly more acute kidney injury compared with non-contrast scans |
|
Qian et al.(6) |
Randomized controlled clinical trial |
394 patients with chronic renal failure and congestive heart failure |
Iodinated contrast in coronary procedures |
Incidence of 12,8 % in the adequate hydration group versus 21,2 % in the control group (P = 0,018) |
Adequate hydration combined with nitrates |
Adequate hydration with nitrates was effective in reducing contrast-induced nephropathy in patients with chronic renal failure and heart failure |
|
Sun et al.(7) |
Meta-analysis |
1916 patients undergoing contrast studies, including patients with chronic renal failure and diabetes mellitus |
Iodinated radiological contrasts for coronary and angiographic procedures |
Non-significant reduction in the risk of contrast-induced nephropathy (relative risk of 0,68, P = 0,06) |
Administration of intravenous N-acetylcysteine to reduce the risk of contrast-induced nephropathy |
No significant benefit of intravenous N-acetylcysteine was demonstrated in reducing contrast-induced nephropathy |
|
Weisbord et al.(8) |
Randomized clinical trial |
4418 patients from 53 medical centers undergoing coronary and non-coronary angiography |
Iodinated contrast in coronary and non-coronary angiographies |
Incidence of 1,2 % of clinically significant post-contrast renal injury at 90 days (death, dialysis, or persistent renal damage) |
Intravenous hydration with isotonic sodium bicarbonate or isotonic sodium chloride, together with N-acetylcysteine |
Post-contrast renal injury was associated with a 3,93-fold increased risk of 90-day mortality, dialysis, or persistent renal damage |
|
Cheungpasitporn et al.(9) |
Meta-analysis |
513 patients undergoing elective procedures with contrast |
Iodinated contrast in elective procedures (oral vs intravenous) |
8,8 % overall incidence of AKI in patients with elective procedures; no significant difference between oral and intravenous hydration regimens |
Oral and intravenous hydration |
There were no significant differences in the incidence of AKI between oral and intravenous hydration in elective patients |
|
Lee et al.(10) |
Clinical study |
5267 patients undergoing diagnostic or interventional coronary angiography |
Low osmolarity and isoosmolar contrast agents (iopromide vs iodixanol) |
Incidence of renal injury of 11,7 % with low-osmolarity contrast agents versus 9,3 % with isosmolar contrast agents |
Isotonic hydration before and after contrast exposure |
No significant differences were found in the incidence of renal injury between low-osmolarity and isosmolar contrast agents |
|
Everson et al.(11) |
Systematic review |
Patients admitted to emergency departments with renal failure or risk factors for acute kidney injury |
Iodinated and isoosmolar contrast for computed tomography and coronary angiography procedures |
Contrast-associated acute kidney injury occurred in 15 % of hospitalized patients |
Use of intravenous hydration and low-osmolarity contrasts to reduce risk |
Renal injury is multifactorial, and patients with chronic renal failure are at increased risk of acute kidney injury |
|
van der Molen et al.(12) |
Systematic review |
57 000 patients (adults and children) undergoing contrast-enhanced procedures |
Intravenous ioversol (low osmolarity) |
Post-contrast renal injury ranged from 1 % to 42 %, with no evidence of an increase with the use of ioversol |
Selection of low-osmolarity contrast media and monitoring of patients with renal insufficiency |
Ioversol showed a safety profile comparable to other contrast agents with a low incidence of adverse effects |
|
Ehrmann et al.(13) |
Systematic review and Bayesian meta-analysis |
1153 patients in the ICU, comparing patients exposed to contrast and those not exposed |
Iodinated contrast agents in critically ill patients (observational with control group) |
The Bayesian meta-analysis found no significant increase in acute kidney injury attributed to contrast in critically ill patients (OR 0,95) |
Intravenous hydration and continuous monitoring of renal function |
No evidence was found that iodinated contrast media significantly increase the risk of acute kidney injury in critically ill patients |
|
Weinreb et al.(14) |
Systematic review |
Patients with advanced kidney disease, including those with acute and chronic renal failure |
Gadolinium-based contrast media (Group II and III) |
The risk of nephrogenic systemic fibrosis is very low for group II contrast agents |
Use of contrast agents from group II is recommended over group I; dialysis is not necessary after administration of group II |
The risk of kidney toxicity with gadolinium-based contrast media of group II is negligible even in patients with severe kidney failure |
|
Honda et al.(15) |
Retrospective cohort study |
42 501 patients undergoing contrast-enhanced computed tomography scans at Osaka National Hospital |
Non-ionic contrast media used in computed tomography |
Incidence of serious adverse reactions of 0,019 %, including two deaths |
Premedication with corticosteroids and monitoring to reduce adverse reactions |
Serious adverse reactions related to non-ionic contrast media are rare but can be life-threatening |
|
Cha et al.(16) |
Multicenter study with statistical analysis |
196 081 patients undergoing contrast-enhanced procedures with iodinated contrast media |
Iodinated contrast media in computed tomography |
Overall prevalence of hypersensitivity reactions of 0,73 %; serious reactions in 0,01 % of cases |
Premedication with antihistamines and change of contrast medium to prevent recurrent reactions |
A previous history of hypersensitivity to contrast media and the presence of allergic diseases are key risk factors |
|
Gomi et al.(17) |
Prospective controlled study |
513 patients undergoing elective contrast-enhanced procedures |
Five low-osmolar non-ionic contrast media |
8,8 % overall incidence of AKI in patients undergoing elective procedures; no significant difference between oral and intravenous hydration regimens |
Selection of contrast media with a lower rate of adverse reactions, such as iopamidol, iohexol, and ioversol |
Iomeprol and iopromide are associated with a higher incidence of acute adverse reactions compared to other contrast media |
Frequency of Contrast-Induced Nephropathy
Several studies have examined the frequency of contrast-induced nephropathy, observing differences depending on the type of contrast medium used and the condition of the patients. For example, one study found that the risk of developing nephrogenic systemic fibrosis with the use of Group II gadolinium-based contrast media was extremely low, even in patients with severe renal impairment. No cases of this complication were reported in patients with advanced kidney disease treated with Group III agents.(14)
Similarly, another study documented that the frequency of severe adverse reactions to using non-ionic contrast agents in computed tomography was minimal, at just 0,019 %. Despite this, two deaths were reported among 42 501 patients studied.(10) A larger analysis, which included 196 081 patients undergoing procedures with iodinated contrast media, reported an overall prevalence of hypersensitivity reactions of 0,73 %, of which the most severe affected only 0,01 %.(15) Another prospective study of 8931 patients showed that the frequency of acute adverse reactions was 2,7 %, being higher in the groups receiving iomeprol (3,9 %) and iopromide (3,5 %).(16)
On the other hand, another study found no significant differences in the risk of acute kidney injury between patients who received CT scans with or without intravenous contrast.(6)
Comparison of Contrast Media
A comparative study evaluated the differences between low-osmolarity and iso-osmolar contrast media and found no significant differences in contrast-induced acute kidney injury incidence. The rates were 11,7 % for low-osmolarity media and 9,3 % for iso-osmolar press. Still, after adjusting the data using propensity score analysis, the figures were even closer: 9,9 % versus 9,5 %, with no statistical significance detected between the two groups.(12)
One study found no confirmed cases of nephrogenic systemic fibrosis associated with the use of Group II gadolinium-based contrast media in patients with advanced renal failure. These agents were used without reported complications.(14)
Risk Factors and Preventive Strategies
Regarding risk factors and preventive strategies, one study revealed that contrast-induced nephropathy was less frequent in patients with chronic renal failure and congestive heart failure who received adequate hydration with nitrates, with a rate of 12,8 % compared to 21,2 % in the control group.(17)
In addition, 15 % of hospitalized patients with renal failure developed acute kidney injury associated with contrast use. In this context, the importance of intravenous hydration as a key preventive measure was highlighted.(5) Likewise, the contrast media iopamidol, iohexol, and ioversol, which had lower rates of adverse reactions, were preferred in younger patients.(16)
DISCUSSION
This systematic review provides insight into the differences in nephrotoxicity caused by various contrast media, as well as the most effective preventive strategies for patients at risk of developing acute kidney injury. When comparing these findings with previous studies, there is general consistency with the current literature. For example, Group II gadolinium-based contrast agents, such as gadobutrol (Gadovist®), gadoteric acid (Dotarem®), and gadolinium (Prohance®), are safe even in patients with advanced renal impairment, making them a preferred option for this type of patient. These agents have a more stable chemical structure, which reduces the release of free gadolinium into the body and, therefore, the risk of toxicity.(14)
On the other hand, Group III contrast agents, such as disodium gadoxetate (Primovist®/Eovist®), which are mainly used for liver imaging, still require further studies to confirm their safety in patients with renal impairment. So far, they have not been associated with serious adverse effects, but additional research is needed before recommending their use in populations at high risk of nephrotoxicity.
The studies reviewed show a low prevalence of severe adverse reactions in iodinated contrast media. This aligns with multicenter research indicating a minimal incidence of mortality associated with these agents. However, they highlight the importance of careful monitoring and implementing preventive strategies such as intravenous hydration to reduce the risk of contrast-induced acute kidney injury.(10,15) Although studies did not identify significant differences between low-osmolarity and iso-osmolar agents in contrast-induced nephropathy,(12) further research is recommended to determine which is more suitable in higher-risk populations.
Future research should focus on prospective controlled clinical trials, especially in high-risk patients such as those with chronic renal failure and diabetes.(5)
In this review, iso-osmolar contrast agents, such as iodixanol, have shown a similar safety profile, and even superior in some cases, to low-osmolar agents in specific clinical settings.(12,16) This is relevant in clinical practice, where choosing the appropriate contrast medium is essential to prevent contrast-induced acute kidney injury. Although these results are promising, the studies do not allow a definitive conclusion to be drawn as to which agent is safest. Further research is needed to directly compare iso-osmolar and low-osmolar agents in homogeneous populations to guide clinical decisions better.
Another point to note is the variability in the preventive strategies used in the studies, which makes it difficult to extrapolate the results. Although intravenous hydration is considered a key preventive measure, the type of solution and timing of administration vary between studies, which may influence the results obtained.(5) This highlights the importance of establishing a consensus on best preventive practices for high-risk patients.
This systematic review supports the conclusion that Group II gadolinium-based contrast agents have a low-risk profile for nephrotoxicity. It suggests that iso-osmolar agents may offer equivalent or superior safety to low-osmolar agents in certain patient groups.
However, further studies are needed to more accurately assess optimal preventive interventions and the impact of contrast agents in patients with comorbidities such as cardiovascular disease so that strategies can be better tailored to the characteristics of each clinical profile.
CONCLUSIONS
This systematic review showed that, although iodinated and gadolinium-based contrast media remain indispensable tools in diagnostic imaging, their use carries a potential risk of contrast-induced nephropathy (CIN), especially in patients with predisposing factors such as chronic renal failure and diabetes mellitus. Although the overall incidence of CIN has been low, the studies evaluated showed that this risk may increase significantly in vulnerable populations and specific clinical settings.
The findings highlighted the importance of appropriate contrast agent selection, considering that iso-osmolar compounds such as iodixanol may offer a more favorable safety profile than some low-osmolarity agents. In the case of gadolinium-based contrast agents, those in Group II were confirmed as safe even in patients with impaired renal function, while those in Group III still require further evidence to validate their use in high-risk populations.
The review also highlighted the need to implement standardized preventive strategies, with intravenous hydration before and after the procedure being one of the most effective and consistent measures. However, the heterogeneity of interventions and the lack of consensus on the optimal protocol for their administration indicate that further studies are needed to consolidate more uniform clinical guidelines.
In conclusion, this review reaffirmed the need for an individualized and multidisciplinary approach to administering contrast media to maximize their diagnostic benefits while minimizing the associated renal risks.
BIBLIOGRAPHIC REFERENCES
1. Shams E, Mayrovitz HN. Contrast-Induced Nephropathy: A Review of Mechanisms and Risks. Cureus; 2021 May 4. https://www.cureus.com/articles/58401-contrast-induced-nephropathy-a-review-of-mechanisms-and-risks
2. Mamoulakis C, Tsarouhas K, Fragkiadoulaki I, Heretis I, Wilks MF, Spandidos DA, et al. Contrast-induced nephropathy: Basic concepts, pathophysiological implications and prevention strategies. Pharmacol Ther. 2017 Dec;180:99–112.
3. Contrast Media Safety Committee. ESUR Guidelines on Contrast Agents, version 10.0. European Society of Urogenital Radiology; 2018.
4. Gorelik Y, Yaseen H, Heyman SN, Khamaisi M. Negligible risk of acute renal failure among hospitalized patients after contrast-enhanced imaging with iodinated versus gadolinium-based agents. Invest Radiol. 2019 May;54(5):312–8.
5. McDonald RJ, McDonald JS, Bida JP, Carter RE, Fleming CJ, Misra S, et al. Intravenous contrast material–induced nephropathy. Contrast Media. 2013;267(1).
6. Qian G, Liu C, Guo J, Dong W, Wang J, Chen Y. Prevention of contrast-induced nephropathy by adequate hydration combined with isosorbide dinitrate for patients with renal insufficiency and congestive heart failure. Clin Cardiol. 2019 Jan;42(1):21–5.
7. Sun Z, Fu Q, Cao L, Jin W, Cheng L, Li Z. Intravenous N-acetylcysteine for prevention of contrast-induced nephropathy: A meta-analysis of randomized, controlled trials. PLoS One. 2013 Jan 30;8(1):e55124.
8. Weisbord SD, Palevsky PM, Kaufman JS, Wu H, Androsenko M, Ferguson RE, et al. Contrast-associated acute kidney injury and serious adverse outcomes following angiography. J Am Coll Cardiol. 2020 Mar;75(11):1311–20.
9. Cheungpasitporn W, Thongprayoon C, Brabec B, Edmonds P, O′Corragain O, Erickson S. Oral hydration for prevention of contrast-induced acute kidney injury in elective radiological procedures: A systematic review and meta-analysis of randomized controlled trials. N Am J Med Sci. 2014;6(12):618.
10. Lee T, Kim WK, Kim AJ, Ro H, Chang JH, Lee HH, et al. Low-osmolar vs. iso-osmolar contrast media on the risk of contrast-induced acute kidney injury: A propensity score matched study. Front Med. 2022 Apr 29;9:862023.
11. Everson M, Sukcharoen K, Milner Q. Contrast-associated acute kidney injury. BJA Educ. 2020 Dec;20(12):417–23.
12. Van Der Molen AJ, Dekkers IA, Bedioune I, Darmon-Kern E. A systematic review of the incidence of hypersensitivity reactions and post-contrast acute kidney injury after ioversol in more than 57,000 patients: part 1—intravenous administration. Eur Radiol. 2022 Mar 21;32(8):5532–45.
13. Ehrmann S, Quartin A, Hobbs BP, Robert-Edan V, Cely C, Bell C, et al. Contrast-associated acute kidney injury in the critically ill: systematic review and Bayesian meta-analysis. Intensive Care Med. 2017 Jun;43(6):785–94.
14. Weinreb JC, Rodby RA, Yee J, Wang CL, Fine D, McDonald RJ, et al. Use of intravenous gadolinium-based contrast media in patients with kidney disease: Consensus statements from the American College of Radiology and the National Kidney Foundation. Radiology. 2021 Jan;298(1):28–35.
15. Honda T, Kuriyama K, Kiso K, Kishimoto K, Tsuboyama T, Inoue A, et al. Incidence rate of severe adverse drug reactions to nonionic contrast media at the National Hospital Organization Osaka National Hospital. Allergo J Int. 2020 Nov;29(7):240–4.
16. Cha MJ, Kang DY, Lee W, Yoon SH, Choi YH, Byun JS, et al. Hypersensitivity reactions to iodinated contrast media: A multicenter study of 196,081 patients. Radiology. 2019 Oct;293(1):117–24.
17. Gomi T, Nagamoto M, Hasegawa M, Katoh A, Sugiyama M, Murata N, et al. Are there any differences in acute adverse reactions among five low-osmolar non-ionic iodinated contrast media? Eur Radiol. 2010 Jul;20(7):1631–5.
FINANCING
None.
CONFLICT OF INTEREST
Authors declare that there is no conflict of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Aline Aparecida Pacheco, Analía Claudia Sabattini.
Data curation: Aline Aparecida Pacheco, Analía Claudia Sabattini.
Formal analysis: Aline Aparecida Pacheco, Analía Claudia Sabattini.
Drafting - original draft: Aline Aparecida Pacheco, Analía Claudia Sabattini.
Writing - proofreading and editing: Aline Aparecida Pacheco, Analía Claudia Sabattini.