doi: 10.56294/shp2024147
ORIGINAL
Learning needs of general practitioners in the management of acute myocardial infarction with ST segment elevation and pharmacological reperfusion strategies
Necesidades de aprendizaje de médicos generalistas en el manejo del Infarto Agudo de Miocardio con elevación del segmento ST y estrategias de reperfusión farmacológica
Kamylla Dayse Dos Santos Lima1 *, Leandro Rodríguez Pardal1 *
1Universidad Abierta Interamericana, Facultad de Medicina y Ciencias de la Salud, Carrera de Medicina. Buenos Aires, Argentina.
Cite as: Dos Santos Lima KD, Rodríguez Pardal L. Learning needs of general practitioners in the management of acute myocardial infarction with ST segment elevation and pharmacological reperfusion strategies. South Health and Policy. 2024; 3:147. https://doi.org/10.56294/shp2024147
Submitted: 29-08-2023 Revised: 18-01-2024 Accepted: 30-06-2024 Published: 01-07-2024
Editor:
Dr. Telmo Raúl Aveiro-Róbalo ![]()
Corresponding Author: Kamylla Dayse Dos Santos Lima *
ABSTRACT
Introduction: ischemic heart disease is the leading cause of death worldwide. Initial management in primary care centers is associated with early recognition of the condition, as well as the implementation of immediate and effective therapeutic strategies. In this systematic review, the existing empirical evidence was gathered on the learning needs required by recently received general practitioners for the management of acute myocardial infarction with ST segment elevation and its respective pharmacological reperfusion strategy in the primary care of this pathology.
Method: a systematic review of more than 30 articles available from the literature was carried out, including the recommendations of national guidelines (Argentine Society of Cardiology), international guidelines (American Heart Association and European Society of Cardiology) as well as the most medical search engines. relevant for the management of AMI and its pharmacological reperfusion.
Results: in this systematic review, deficits were revealed to include lack of recognition and adequate treatment of AMI symptoms, delays in care, deficiencies in ECG interpretation, and limitations in training in emergency procedures. Although there is a general understanding about the use of certain drugs (such as aspirin and beta- blockers), some physicians are unaware of treatment protocols, also identifying shortcomings in referral strategies and a limited availability of educational resources.
Conclusions: the crucial role that primary care plays in the early identification and management of STEMI symptoms is highlighted. To improve primary care, it is suggested to train staff, implement standardized protocols, and use technology that facilitates diagnosis and treatment. It is essential that health policies prioritize primary care and promote the integration of services to address STEMI more effectively. There is great potential to improve care through collaboration between different sectors.
Keywords: Acute Myocardial Infarction; Primary Health Care; General Practitioners; Health Knowledge; Farmacological Treatment of Myocardial Infarction.
RESUMEN
Introducción: la cardiopatía isquémica es la principal causa de muerte a nivel mundial. El manejo inicial en los centros de atención primaria se asocia al reconocimiento precoz del cuadro, así como la implementación de estrategias terapéuticas inmediatas y eficaces. En esta revisión sistemática se reunió la evidencia empírica existente sobre necesidades de aprendizaje que requieren médicos generalistas recién recibidos para el manejo del infarto agudo de miocardio con elevación del segmento ST y su respectiva estrategia de reperfusión farmacológica en la atención primaria de esta patología.
Método: se realizó una revisión sistemática de más de 30 artículos disponibles de la literatura, incluyendo las recomendaciones de las guías nacionales (Sociedad Argentina de Cardiología), internacionales (American Heart Association y European Society of Cardiology) así como los buscadores médicos más relevantes para el manejo del IAM y la reperfusión farmacológica del mismo.
Resultados: en esta revisión sistemática, se revelo que los déficits incluyen la falta de reconocimiento y tratamiento adecuado de los síntomas del IAM, demoras en la atención, deficiencias en la interpretación del ECG y limitaciones en la capacitación en procedimientos de emergencia. Si bien hay un entendimiento general sobre el uso de ciertos fármacos (como aspirina y betabloqueantes), algunos médicos desconocen los protocolos de tratamiento, identificándose además falencias en las estrategias de derivación y una escasa disponibilidad de recursos educativos.
Conclusiones: se resalta el papel crucial que juega la atención primaria en la identificación temprana y el manejo de los síntomas de IAMCEST. Para mejorar la atención primaria, se sugiere capacitar al personal, implementar protocolos estandarizados y utilizar tecnología que facilite el diagnóstico y tratamiento. Es esencial que las políticas de salud prioricen la atención primaria y promuevan la integración de servicios para abordar el IAMCEST de manera más efectiva. Existe un gran potencial para mejorar la atención mediante la colaboración entre diferentes sectores.
Palabras clave: Infarto Agudo de Miocardio; Atención Primaria; Médico Generalista; Conocimientos en Salud; Tratamiento Farmacológico del IAM.
INTRODUCTION
The diagnosis and treatment of acute myocardial infarction (AMI) begins at the point of first medical contact, which is defined as the point at which the patient receives primary care from a professional in a prehospital (usually outpatient) setting. Early recognition of ST-segment elevation AMI is necessary to implement effective reperfusion treatment in order to avoid complications and reduce morbidity and mortality since cardiovascular disease remains the leading cause of death worldwide.(1,2,3)
In primary care for AMI, it is essential to recognize symptoms quickly and activate reperfusion processes. Timely and effective care at this stage makes a difference, improving patient survival.(4,5,6)
The importance of identifying and treating AMI appropriately lies in the fact that it is a serious medical condition that can be life-threatening if not addressed quickly and effectively. Identifying the symptoms of AMI and acting promptly can mean the difference between life and death.(7,8,9)
The inability of general practitioners to correctly diagnose and treat AMI is a complex issue involving factors such as academic training, clinical practice, and even the health facility where they work. A lack of resources or poor infrastructure can hinder proper diagnosis.(10,11,12)
In a study by the Jordan University Hospital in Malaysia, 60 % of participants had a bachelor's degree; a survey was conducted to assess healthcare professionals' knowledge of managing acute myocardial infarction (AMI) in a hospital setting.(13,14,15) Most of them demonstrated knowledge and experience in this field. For example, 63,1 % of respondents recognized that an electrocardiogram (ECG) is essential for diagnosing and locating AMI. In addition, 41,54 % of participants could interpret the ECG to detect ST segment elevation correctly.(16)
The study also revealed that 60,54 % of participants understand that patients with myocardial infarction should receive long-term treatment with aspirin, beta-blockers, statins, and ACE inhibitors. Furthermore, 47,21 % knew that if a patient develops sinus bradycardia after an AMI, physicians should increase the heart rate with atropine only if the patient is hemodynamically stable. Although healthcare professionals generally know AMI management, many lack fundamental skills and experience.
The emergence of new technologies highlights the need for a deeper understanding of AMI, its diagnosis, and treatment techniques.(17,18) Specifically, hospitals in developing and developed countries do not yet have full access to these advanced technologies for treating AMI.(19) Limited access to educational resources prevents professionals from improving their knowledge and providing effective treatment.(20) The research found that, of 65 healthcare professionals surveyed, 78,46 % agreed that the scarcity of educational resources limited their ability to receive additional training in AMI management.
While most have basic knowledge, it is clear that they need to deepen their understanding of various interventions and management techniques. This study revealed that 47,69 % of the 65 respondents did not know that AMI is caused by a complete occlusion of the coronary vessels resulting from a thrombus, which is reflected in ST-segment elevation on the ECG. However, the study also found that, in general, these professionals had a good knowledge of pharmacological interventions. Therefore, training should focus on collaboration, access to technology, performing emergency procedures, and understanding lifestyle modifications and therapies.
In another study on medical education after COVID-19 and the rise of the online learning era, medical educators sought remote teaching methods to provide solutions that allowed teaching to continue during the COVID-19 pandemic. Cardiovascular learning involves the acquisition of knowledge and skills that are typically based on contact learning. However, there are significant gaps in the published literature on the feasibility, effectiveness, and learning outcomes of different remote learning methods.
A study conducted in the Merseyside region of England revealed that, out of 150 physicians, only 82 % were able to correctly diagnose AMI from ECG interpretation. This indicates the need for ongoing training for these professionals. Finally, all primary care facilities should have ECG centers, including those located in remote areas.(21)
As the first point of contact, general practitioners must know when to refer a patient with chest pain. Physicians must have ECG monitoring and interpretation skills. Therefore, it is recommended that these skills be taught in the undergraduate curriculum.
A performance assessment was conducted of 771 candidates aspiring to enter directly into the Hospital Clinical Medicine Residency Program at FMRP-USP. This assessment was carried out in a simulated AMI setting, with the participation of professional actors and medical evaluators, using a standardized checklist. The average age of the participants was 25 years (range 24 to 27), and 58 % were men. The vast majority (90 %) were newly graduated physicians, 71 % had graduated less than a year earlier, and 19 % between one and two years earlier. In addition, 66 % of the candidates came from public universities.
Regarding the specific actions on the checklist associated with treatment, the following results were observed: 83 % of applicants requested ECG monitoring, 57 % indicated the insertion of a peripheral venous access device, 95 % administered acetylsalicylic acid, 80 % added a second antiplatelet agent (P2Y12 inhibitor), 66 % administered sublingual nitrates, and 71 % administered intravenous morphine for pain control. Sixty-nine percent correctly identified the diagnosis of STEMI, while 28 % recognized the infarction but did not mention ST-segment elevation. The duration of pain was recorded by 71 % of applicants.
Most applicants (63 %) recognized the need to transfer the patient for reperfusion, although only 19 % specified the reason for transfer (reperfusion therapy), and 18 % did not mention the need for transfer at all. Only 25 % insisted on transfer to a tertiary center, even if no beds were available after the actor's intervention. Four percent of callers waited for myocardial necrosis markers before deciding on the treatment to follow.
Another study, which interviewed 97 patients who suffered an acute myocardial infarction, revealed that only 33 % were hospitalized immediately, while 67 % had to go to several units before being admitted. Among the main reasons for not being hospitalized, it was noted that doctors did not identify the diagnosis, sending patients home. In addition, when standardized questionnaires were administered to medical students, it was found that only 22 % knew how to assist patients with myocardial infarction.
Pharmacological reperfusion strategies
The latest Argentine Consensus highlights several barriers that hinder early reperfusion in patients with STEMI:
· Time to PCM (First Medical Contact): patients must recognize the symptoms of an AMI and know how to contact the emergency services. To facilitate this communication, a single telephone number and trained personnel should be implemented.
· Delay in diagnosis: the diagnosis should be made in less than 10 minutes from the patient's arrival at the institution. This requires electrocardiographs in ambulances and a priority admission system in emergencies to attend to suspected AMI cases quickly. ECG teletransmission before hospitalization can speed up management and increase the likelihood of timely reperfusion.
· Delay in reperfusion treatment: this time reflects the efficiency of the healthcare system and is a predictor of clinical outcomes. A shorter time to reperfusion treatment is associated with better outcomes, including less myocardial necrosis and lower mortality.
Summary of recommendations for the management of STEMI
This set of recommendations seeks to improve the management and prognosis of patients with STEMI, prioritizing rapid and effective interventions.
1. Immediate Electrocardiogram: all adults with acute chest pain should undergo a 12-lead ECG within the first 10 minutes to detect STEMI and allow for early reperfusion therapy.
2. Immediate Aspirin: to reduce mortality and morbidity, it is recommended that 150–325 mg of aspirin be administered orally or 250–500 mg intravenously to all adult patients with chest pain consistent with STEMI, even if they arrive late.
3. Reperfusion therapy: early reperfusion therapy should be implemented in patients diagnosed with STEMI within 12 hours of symptom onset.
4. Preference for PTA: this should be preferred over fibrinolysis for those who can receive primary angioplasty (PTA) in less than 120 minutes.
5. Fibrinolysis if PTA is unavailable: if PTA cannot be guaranteed within 120 minutes, immediate fibrinolysis should be administered.
6. Late reperfusion: late reperfusion therapy (preferably PTA) should be considered for patients who present more than 12 hours after symptom onset and have hemodynamic decompensation.
7. Prehospital fibrinolysis: in patients with STEMI diagnosed by mobile emergency services, immediate prehospital fibrinolysis is recommended if ATCp cannot be guaranteed within 120 minutes.
8. Transfer to treatment centers: patients who cannot receive ATCp or prehospital fibrinolysis should be transferred to centers where appropriate treatment can be administered.
9. Rescue ATC: in patients without reperfusion criteria after fibrinolysis, immediate referral for rescue ATC should be made.
10.Do Not Repeat Fibrinolysis: if there are no reperfusion criteria, a new dose of fibrinolytic should not be administered, as this increases the risk of bleeding.
11.Pre-Discharge Echocardiogram: an echocardiogram is recommended for all patients with STEMI before discharge to assess the size of the infarction and ventricular function.
12.Chronic Aspirin: low-dose aspirin therapy is suggested for patients with coronary artery disease to prevent new events.
13.High-intensity statins: high-intensity statins are recommended to reduce the risk of cardiovascular events in patients with cardiovascular disease.
14.Smoking cessation: patients should be asked about their tobacco use and offered effective smoking cessation interventions, given their high risk after an AMI.
An uncomplicated STEMI occurs without signs or symptoms of acute heart failure, mechanical complications, or significant arrhythmias. After electrocardiographic confirmation of ACS with ST-segment elevation, the emergency services should be activated, according to each individual scenario at the first point of contact. General management measures include:
· Place the patient in complete rest with the head elevated and, if possible, weigh them beforehand.
· Monitor vital signs: blood pressure, heart rate, and oxygen saturation. Non-invasive blood pressure monitoring every 5 minutes, monitoring with the possibility of defibrillation or electrical cardioversion
· Insert at least two peripheral intravenous lines with a 16 G or 18 G Abbocath, avoiding flexion of the elbow (antecubital line), preferably in the left forearm. Avoid placing a central intravenous line, intramuscular line, or Foley catheter.
· Blood sampling for routine laboratory tests without delaying the start of treatment or transfer. All patients are advised to request a complete blood count, glucose, urea, creatinine, liver profile, lipid profile, coagulation profile, glycosylated hemoglobin, blood type and RH factor, troponin, CPK-MB (in the absence of troponin). The reperfusion strategy chosen for each patient will depend on the time of symptom onset, the availability of resources at each center or network, and the estimated time to reperfusion
Delays in reperfusión
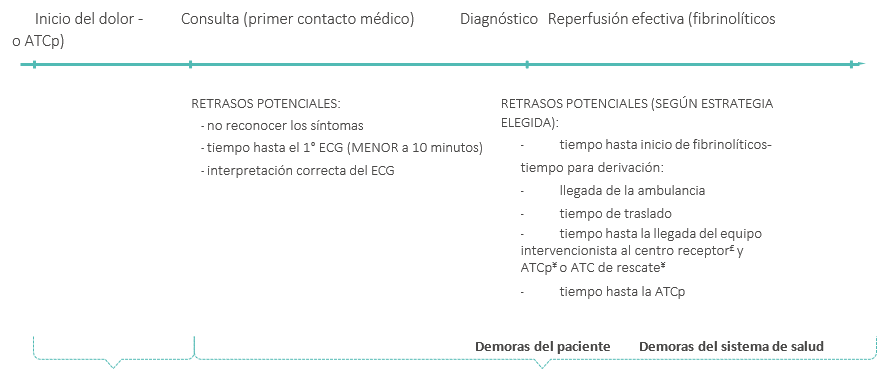
Figure 1. Delays in care at the IAMCEST
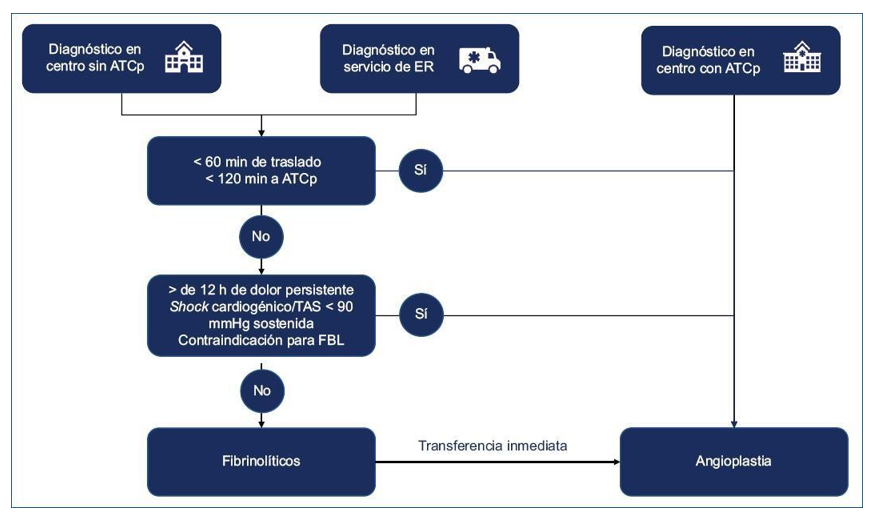
Figure 2. Algorithm for reperfusion therapy decision. PCI: primary coronary intervention; ER: emergency room; FL: fibrinolytics; SBP: systolic blood pressure
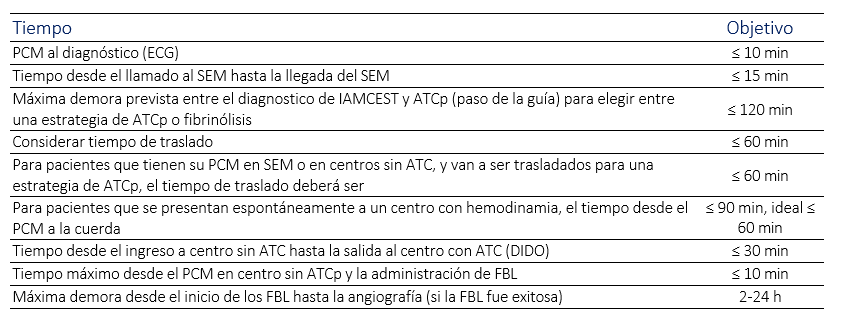
Figure 3. Recommended times for treating patients with STEMI
METHOD
During the first stage, a protocol was developed to ensure the method's transparency. This protocol was presented to and approved by the committee responsible for this task. A systematic review of the available literature was carried out, including recommendations from national (Argentine Society of Cardiology) and international (American Heart Association and European Society of Cardiology) guidelines, as well as the most relevant medical search engines for the management of AMI.
A systematic review of the available literature was conducted, including recommendations from national guidelines (Argentine Society of Cardiology), international guidelines (American Heart Association and European Society of Cardiology), and the most relevant medical search engines for managing AMI by primary care physicians. More than 15 articles were found on deficits in treating STEMI in primary care, and more than 24 000 articles on pharmacological approaches.
RESULTS
This systematic review revealed that the deficits presented by newly graduated physicians in the management of acute myocardial infarction (AMI), according to the text, are as follows: There is a lack of ability to identify the symptoms of AMI. One study showed that only 22 % of the physicians surveyed could correctly identify an AMI. However, some have basic knowledge about the importance of the electrocardiogram (ECG); a significant percentage do not know how to correctly interpret it to detect ST-segment elevation, which is crucial for diagnosing AMI. Many physicians lack skills and experience in performing emergency procedures related to AMI treatment. While there is a general understanding of the use of certain drugs (such as aspirin and beta-blockers), some physicians are not familiar with long-term treatment protocols or the appropriate interventions based on the patient's condition.
A lack of educational resources and continuing education has been identified as a significant barrier limiting physicians' ability to improve their knowledge and skills in AMI management. Problems with response times, from diagnosis to administration of reperfusion therapy, have been identified, which can negatively impact morbidity and mortality. Many physicians do not adequately specify the need to transfer patients to centers that can perform advanced treatments. A significant percentage do not understand that AMI is caused by complete occlusion of the coronary vessels, underscoring the need for more robust training in this area. This highlights the need for significant improvement in training newly graduated physicians in the management of AMI.
DISCUSSION
There are significant gaps in the published literature on the doctors who graduated during the pandemic regarding the feasibility, effectiveness, and learning with different remote methods. This is a critical point for reflection for the next generations of doctors who will graduate during this period.
Another point is that students and physicians must strengthen their knowledge. That is, they must consider that this is a recurring pathology in everyday life and that it is also horizontal to several others. It is of great importance to know how to manage it well, regardless of whether cardiology is the professional's vocation or not.
CONCLUSIONS
The crucial role of primary care in the early identification and management of STEMI symptoms is highlighted, as well as how strengthening primary care could improve health outcomes. The lack of adequate resources and protocols in primary care can contribute to delays in diagnosis and treatment, which increases associated mortality and morbidity.
Some strategies to improve primary care include training staff, implementing standardized protocols, and using technology to facilitate diagnosis and treatment. Health policies must prioritize primary care and promote the integration of services to address STEMI more effectively. Policymakers, health professionals, and the community must collaborate to close gaps in primary care and improve outcomes for patients with STEMI. Effective interventions and collaboration between different sectors have great potential to improve care.
BIBLIOGRAPHIC REFERENCES
1. Gagliardi JA, Charask A, Perna E, D'Imperio H, Bono J, Castillo Costa Y, et al. Encuesta nacional de infarto agudo de miocardio con elevación del ST en la República Argentina (ARGEN-IAM-ST). Rev Argent Cardiol. 2016;84(6):Ciudad Autónoma de Buenos Aires.
2. Adaro D, Celeste V, Alvarado Giménez JS, Morales IL, Vega GG, Gagliardi J, et al. Revista del Consejo Argentino de Residentes de Cardiología. 2021;(pág. 162):Argentina.
3. Bancos Salud. Actualizaciones de médicos de primer nivel. Argentina: bancos.salud.gob.ar; 2020 jun. https://bancos.salud.gob.ar/sites/default/files/
4. Kusmana D. Role of general practitioner in the management of acute myocardial infarction. Med J Indones. 1999;14(4).
5. Bridgwood B, Cezar S, Houghton J, Andrew N, Coral P, Sayers R. Medical education in a post COVID-19 era: remote teaching methods for cardiovascular knowledge and skills. MedEdPublish. 2021 Mar;10(62).
6. Piombo C, Rolandi F, Fitz MM, Salzberg SI, Strumminger, Custodio-Sánchez P, Miranda-Noé D, López-Rojas M. Propuesta de manejo inicial del infarto de miocardio con elevación del segmento ST no complicado en centros sin capacidad de intervención coronaria percutánea en el Perú. Arch Peru Cardiol Cir Cardiovasc. 2023 Oct–Dec;4(4):164–83.
7. Delgado-Acosta H, Pedraza-Alejo D, Valladares-Carvajal F, Lastre-Navarro K, Hernández-Torres L, Ávila-Piña D. Calidad de la atención médica a pacientes con infarto agudo. Cienfuegos 2011. Rev Finlay. 2013.
8. Fernández HE, Bilbao JA, Cohen Arazi H, Ayerdi ML, Telayna JM, Duronto EA, et al. Registro Multicéntrico SCAR: Rev Argent Cardiol. 2014;82(5):Ciudad Autónoma de Buenos Aires.
9. Fady Y, Zainah M, Gurbinder Kaur JS, Nor Haty H. Identifying educational needs and knowledge gaps in healthcare professionals for effective management of acute myocardial infarction. 2024 Jun;11(6):37–43.
10. Weston CFM, Penny WJ, Julian DG, on behalf of the British Heart Foundation Working Group. Guidelines for the early management of patients with myocardial infarction. BMJ. 1994 Mar 19;308.
11. Folgarait A. Radiografía del infarto en la Argentina. Sociedad Argentina de Cardiología. 2016 nov 7.
12. Fumagalli J, Monsalvo M, Gaglio R, Gil A, Koren L. Ministerio de Salud. Resolución 256. Buenos Aires, AR: 2013 oct 14.
13. Smolderen KG, Spertus JA, Nallamothu BK. Health care insurance, financial concerns in accessing care, and delays to hospital presentation in acute myocardial infarction. JAMA. 2010;303(14):1392–400.
14. Solla RI, Bembibre Vázquez L, Freire Corzo J. Actualización de “ABCDE en Urgencias Extrahospitalarias”: Manejo del síndrome coronario agudo en urgencias de atención primaria. Cad Aten Primaria. 2011;18:49–55.
15. Costabel JP, Quintana M, Perea J, Lamelas P. Documento de posición sobre la mejoría de la reperfusión del IAMCEST en Latinoamérica. Arch Cardiol Méx. 2024 abr-jun;94(2):Ciudad de México.
16. Pourmand A, Tanski M, Steven D, Hamid S, Raymond L, Fareen Z. Educational technology improves ECG interpretation of acute myocardial infarction among medical students and emergency medicine residents. 2015 jan.
17. Rosende A, García Zamora S, Venentini N. Guía de práctica clínica nacional para la reperfusión del infarto agudo de miocardio. Ministerio de Salud; 2020. Argentina.
18. Stocco Aimoli U, Miranda CH. Competence in ST-segment elevation myocardial infarction management by recently graduated physicians applying for a medical residency program. Arq Bras Cardiol. 2020 ene;114(1).
19. Varela García RJ, Olivera Escalona ÁL, Guarton Ortiz OM, Est Dariannis VI, M. Necesidades de aprendizaje de médicos de atención primaria sobre reperfusión coronaria en el infarto agudo del miocardio. Medisan. 2019 mar-abr;9:3–10.
20. Ayanian JZ, Hauptman PJ, Guadagnoli E, Antman EM, Pashos CL, McNeil BJ. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med. 1994 Oct 27;331(17).
21. Zylbersztejn H, Rubio E, Ulmete E, Mitelman PDPJ. Registro de calidad de atención del infarto agudo de miocardio en los hospitales públicos de la ciudad de Buenos Aires. Rev Argent Cardiol. 2010 mayo 17;79(2).
FINANCING
None.
CONFLICT OF INTEREST
None.
AUTHORSHIP CONTRIBUTION
Conceptualization: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Data curation: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Formal analysis: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Research: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Methodology: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Project management: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Resources: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Software: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Supervision: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Validation: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Visualization: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Writing – original draft: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.
Writing – review and editing: Kamylla Dayse Dos Santos Lima, Leandro Rodríguez Pardal.